Coach, should I be on a low carb diet? Part 2: The Test
Alan Couzens, M.S. (Sports Science)
April 7th, 2015
In my last article, I looked at the general applicability of a ketogenic (low carb, high fat) diet for athletes. I suggested that following a LCHF diet when it’s not needed may lead to the very insulin resistance that the athlete is trying to avoid.
To recap: Low carb diets for athletes are in vogue right now, largely due to the work of Dr. Tim Noakes. I am not arguing with Dr. Noakes' assertion that athletes with insulin resistance (I.R.) should adopt a low carbohydrate nutritional strategy. What I am arguing with is the prevalence of true insulin resistance among athletes, or at least the athletes who will be reading this blog - i.e. folks who specialize in events that challenge their metabolic fitness on a daily basis!
So, in this post, I want to take it out of the realm of the theoretical and endeavour to help you answer the simple, but all important question...
... are you an insulin resistant athlete?
So how do we identify if you are insulin resistant and in need of a low carb, ketogenic diet? Answer: We test!
The extreme of insulin resistance – diabetes, is often diagnosed with a particular type of testing called the Glucose Tolerance Test. Given the widespread availability of glucometers (blood sugar test units), it seems prudent to ask: Why wait until something is wrong before we test? An athlete who has an interest in their own health (i.e. ALL athletes) can and should test their blood glucose response on a frequent basis.
In performance terms, for long course/ultra athletes (i.e. athletes in metabolically limited events) blood glucose testing during training is an incredibly powerful tool in fine-tuning the ‘right’ amount (& timing) of CHO input and energy output. I’ll talk about that application in a future post but, in line with my overall philosophy to put health first, I'll start with the health benefits of GTT testing today.
In my previous post, I touched on the negative effects of persistently elevated blood glucose. In addition to all of the health consequences associated with diabetes, high blood glucose has been linked to cardiovascular disease, cancer and just about every other major serious health disorder of modern times. Just this morning I saw this article pop up on my twitter feed
What does sugar do to your brain? A @HuffingtonPost article: http://t.co/8gjlDY6TfF Original research paper here: http://t.co/CVoDeXKQdE
— Journal Physiology (@JPhysiol) April 7, 2015Yes, there is growing support for the relationship between insulin resistance and impaired cognitive function. This extends all the way to Alzheimer’s!
In short, insulin resistance: No Bueno! As human beings, we want to do all that we can to keep our insulin response system in tip top shape. I suggested in my last piece that bypassing it entirely by using ketones in place of glucose may not be the best way to do this! In fact, it may lead to the very insulin resistance that we're looking to avoid! It’s my position that the best route to metabolic health is to take in the right amount of carbohydrate (in accordance with your expenditure) to maintain homeostasis. This extends beyond a theoretical construct. We can actually view this homeostatic response with a glucose tolerance test!
Here’s what you’ll need…
- 1x Glucometer, e.g. http://amzn.to/1ybkmuL
- Test strips.
Here’s what you’ll do…
On a rest day, upon waking, take a baseline glucose measure, then take in 75g of simple sugar dissolved in a liter of water. Ideally in the form of glucose which you can buy at any pharmacy (but a non malto/dextrose based sports drink would also work).
Continue fasting & take a blood glucose readings (ideally*) at the following intervals
- 30 min post
- 60min post
- 2hrs post
- 3hrs post
- 4hrs post
- 5hrs post
- 6hrs post
*Once you’ve got data from a full test, frequent shorter tests (2-3hrs) can be more practical.
And you’ll plug the results into the following spreadsheet.
You’ll see the upper and lower bounds for a ‘normal’ response (from Seale Harris) already marked. You can see how your own response compares as you enter your data in the boxes.
There are 3 faulty responses that you may see. For what it’s worth, I have seen all 3 in low carb athletes.
1. Insulin Resistance
The first is a pattern of traditional insulin resistance, where blood glucose remains elevated (above the normal line) for an extended period of time. Shown below….
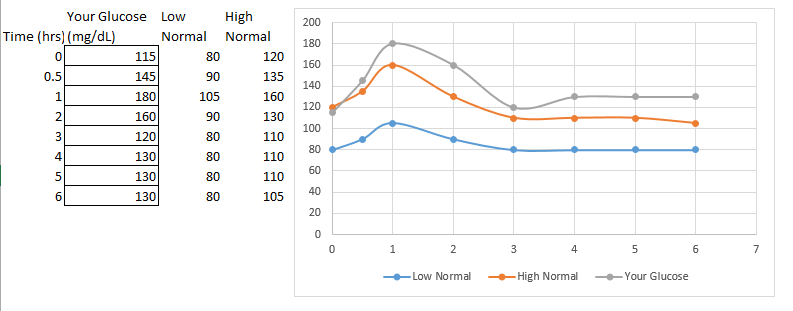
If you are on a normal diet & you are seeing this pattern, it indicates a problem with your glucose regulating system, either a lack of secretion of insulin in response to elevated blood glucose or a resistance to that insulin secreted by the uptake cells. In this case, you are likely insulin resistant and your best bet is probably to significantly decrease the amount of sugar intake because your body is simply not equipped to handle it. If you’re currently on a normal diet & you see this, you are likely to benefit from a low carbohydrate approach.
2. Reactive Hypoglycemia
The second is a pattern of reactive hypoglycemia, where insulin response is there but is not well refined, dare I say, ‘well trained’.
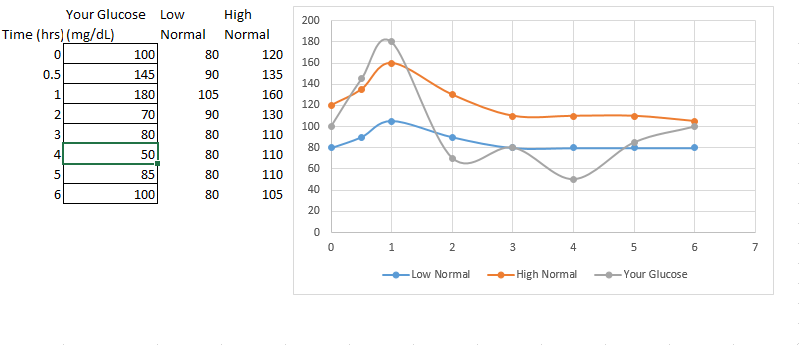
Here we see high glucose initially followed by a blood sugar crash and often times a rebound, as the body bounces back and forth in search of that homeostasis.
We've all experienced this at some point when we overdo it a little e.g. Thanksgiving dinner? :-) Generally it takes significant amounts of CHO to elicit this response. The exception might be in somebody adopting a low CHO approach when not needed, at which point, his system 'forgets' what to do with CHO and even relatively small amounts lead to this response. He becomes a CHO 'lightweight'
Despite lower net glucose, in health terms, this situation is no better than the first. Any insulin dependent diabetic will tell you, it’s not the hyperglycemia that will kill you (at least in the short term), it’s the hypoglycemia that can occur if you get your insulin dosage just a little off. Additionally for long course athletes, not having a blood sugar crash every time you take in CHO is a very good thing! In these cases, ‘training’ the system with manipulations in the glycemic index of the carbs you ingest and activity/stress around meal time may be in order. Highly stressed individuals - folks with habitually elevated gluco-corticoids often exhibit this response
3. Low Response
The third, which is of particular significance to athletes is a ‘flat’ curve, i.e. the body is non-responsive to the stressor. Shown below
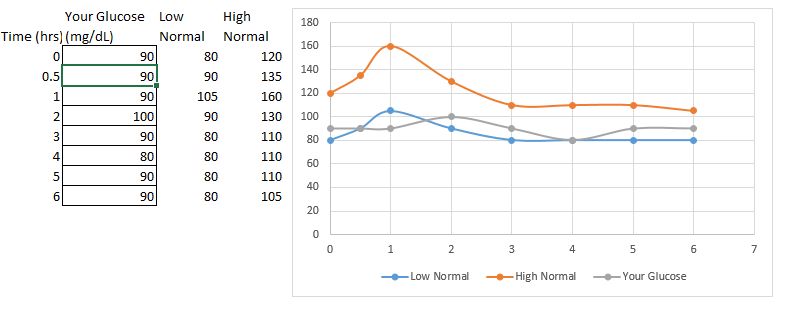
This has hormonal implications which tie in with overtraining & with inadequate carbohydrate consumption for the training load. This type of curve is seen in hypo-adrenergic individuals, i.e. folks whose adrenals are shot. Folks who have a hard time mounting a response to any stressor. Over the short term, this may be an over-reached athlete who is parasympathetically/anabolically dominant - resting insulin is high and the body is primed to immediately take up any sugar that hits the system. This pattern has direct implications on the need for CHO intake.
########
Getting the ‘just right’ amount of insulin response in accordance with blood glucose ‘challenges’ is absolutely critical to survival. So critical that some might argue, it should be trained!
So, what do we do if your GTT is less than ideal?
Well, number 1, have a conversation with your Doctor to rule out any clinically significant deviations from the norm – e.g. Diabetes.
Number 2 – begin to use that glucometer proactively as a biofeedback tool to learn more about your own metabolism….
- Does your response become more ‘normal’ if you eat sweet potato vs regular potato?
- Do you get a better response if you practice relaxation in and around your meal time?
- Most Importantly – do you get a response closer to the ‘normal’ curve on a low carb diet, a moderate carb diet or a higher carb diet?
- And, finally, what role does exercise play? What if you go for a 30min walk after eating? How does your personal response change if you’re eating high carb after a 6 hour ride vs after 6 hours of ‘couch surfing’? I’m going to explore this relationship more in future posts because glucose metabolism in and around exercise is absolutely critical for serious athletes.
But for now, grab a glucometer and play! Blood glucose is such an important bio-marker of health that you should be intimately in touch with your own!
Live smart,
AC
Tweet**************************
Don't miss a post! Sign up for my mailing list to get notified of all new content.
**************************