Cardiac arrhythmias in athletes:
My experience
April 2 2019
As you can probably gather by now, I am a big fan of employing regular HRV (heart rate variability) measurement as a means to prevent over-training and better guide the training prescription for the athletes I work with. I've been doing this for almost a decade now. Over that time, I've had the good fortune to work with some very high level, World Class, endurance athletes and, in addition to the usefulness with regards to health and overtraining, monitoring HRV in this very elite sample has yielded a surprising and important discovery: Cardiac arrhythmias in elite endurance athletes are VERY common!
Without getting into specifics (and potential HIPAA hot water :-) at a certain level of athlete, I would almost go so far as to say that seeing indications of a-fib show up in an athlete's HRV data is not unexpected. And, while it seems to appear more frequently in the elite, this malady isn't restricted to World Class athletes...
In the middle of December, I became a little too personally familiar with Cardiac arrhythmias in athletes. After an unexpected episode of syncope (i.e I passed out and banged my head on the bathroom floor), a routine EKG revealed that I was in atrial fibrillation and so my own journey with cardiac arrhythmias began.
Atrial fibrillation is the most common arrhythmia (both generally and in athletes). It occurs (as displayed in the above gif) when the normal sinus rhythm of the heart is 'short circuited' by some electrical interference from cells that should not be producing their own electrical impulse. You can see these on the gif, quite accurately, as little sparks arising at the base of the pulmonary veins coming into the left atrium. When this happens, rather than the message to beat getting started by the sinoatrial node at the top of the right atrium and then being transferred nicely down the chain(as in the 'normal' illustration), the heart muscle gets mixed messages from various locations and, unsure what to make of it, the signals get bounced around like a pinball machine and the atria just quivers in place. This means that the ventricles don't get the normal delivery of blood from the atria and so the stroke volume is diminished and the heart must work harder by increasing its rate to keep up with the O2 demand. More seriously, over time the pooling of stagnant blood in the atria can lead to blood clots and the potential for Stroke.
While atrial fibrillation is relatively rare, especially in young and middle-age adults, affecting only 0.1% of the population under 50 years of age, recent studies have confirmed my own experience that the incidence of atrial fibrillation is significantly increased in athletes with a long history of endurance training. For example, This meta-analysis showed a 5x greater risk for the development of a-fib in athletes vs non-athletes. In one of the cited studies - the REGICOR study, a dose-response relationship was examined and it was concluded that 1500 hours of lifetime exercise increased the risk of AF by a factor of 3! My experience would cause me to believe that this risk factor continues to scale with lifetime aerobic exercise and by the time we get to top athletes with 10,000+ hours of lifetime aerobic training behind them, the probability of a-fib is significantly increased. While I certainly don't put myself in the same class as many of the athletes I have worked with exhibiting AF, if I'm to add up my own total training volume over the past 30 years of competitive swimming, then running, then triathlon, I suspect the figure is somewhere around 20,000 hours of aerobic load. At an average of ~140bpm, that's 168 million beats! It should probably come as no surprise that this kind of workload leaves a mark!
So what sort of a 'mark' does a high lifetime aerobic load leave?
As a part of my work up, I had an echocardiogram test performed to assess the structure of my heart. Common to long term endurance athletes, my heart chambers, especially the ventricles, were enlarged. This is a functional and desirable adaptation for endurance athletes. In fact, it may be one of the most important adaptations in terms of improving performance. Berbalk (1997) showed a near linear relationship between total heart volume and endurance performance, with top level endurance athletes consistently showing total heart volumes in the range of 1.4L and left ventricular mass of ~300g! This is almost double the normal dimensions for an average untrained heart! While my ticker was certainly not *that* large, I was outside the normal range & this stretching and remodeling may play a role.
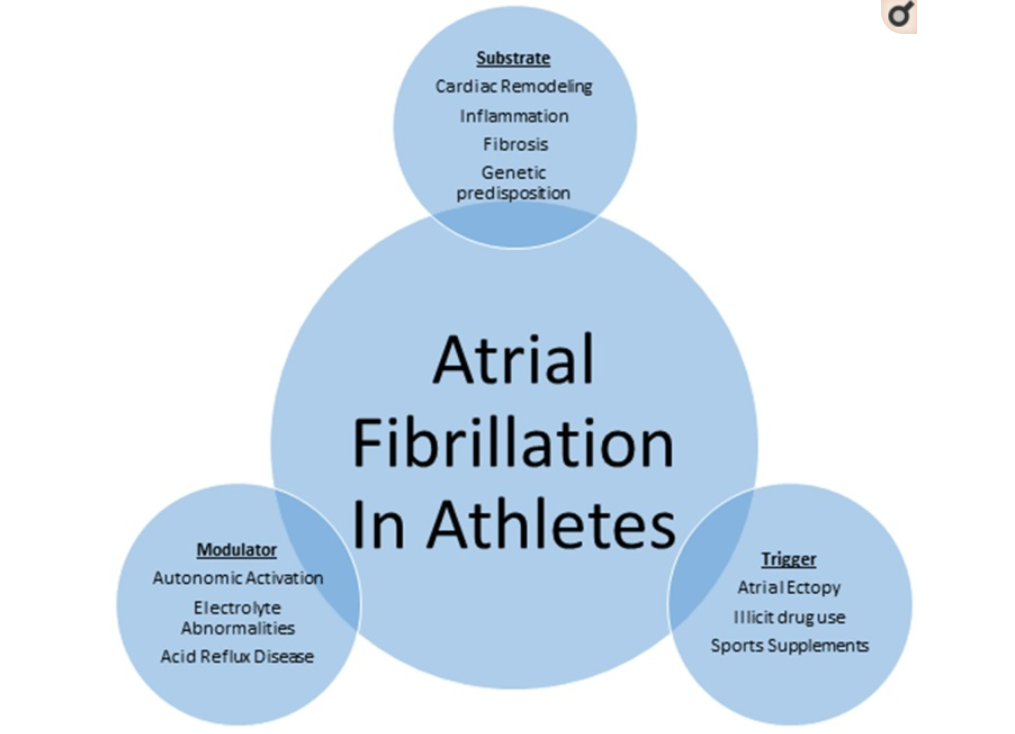
Turagam et al. (2015) does a nice job of summarizing the factors involved in a-fib in athletes in the above chart. And, sure enough, at the very top of the chart the changes to the 'substrate' (i.e. remodeling, inflammation and fibrosis of the heart muscle) induced by training play a large role.
Benito et al. (2010) confirmed this relationship between cardiac fibrosis (caused by atrial dilation) and the incidence of cardiac arrhythmias. Cardiac muscle, like any muscle when stretched, goes through a remodeling/healing process as it adapts to the load. If this healing is incomplete, it can leave behind fibrous tissue which will not do a good job conducting the electrical signals from the sinoatrial node in the way it is supposed to, leading to the potential for 'short circuiting' mentioned above. Mont et al. 2008 also backed up the important role of chamber remodeling in a-fib by finding that atrial dilation, i.e. 'stretched' atrial chambers were strongly correlated with the incidence of a-fib. As I mentioned above, 'stretched' chambers are very common in athletes. Pelicia et al, found that large atrial diameter (>29.0mm/m2) was present in 83% of athletes with more than 4500 hours of lifetime training vs only 24% in those with less than 1500 hours of lifelong training. With atrial dilation being an important factor in the development of arrhythmias and atrial dilation occuring at 4x the rate in athletes with more than 4500 hours of lifelong training, it should come as little surprise that the risk of a-fib tends to scale with hours of endurance training.
An additional, and interesting contributing factor, from the chart above, is another adaptation that we very much desire as endurance athletes. Activation of the autonomic nervous system, specifically the Vagal branch, may serve an important role as a modulator of A.F. In other words, it turns out those high HRV numbers may not be our friend when it comes to arrhythmias! Coumel (1994), interestingly, identified *increased* vagal tone as a primary factor in a-fib. The mechanism for this seems to be related to the ability of a strong Parasympathetic system to 'put the brakes on': Under normal circumstances, the sympathetic system has a strong influence on heart rate. It is thought that the increased parasympathetic drive seen in endurance athletes may may be overwhelming the influence of the sympathetic system on the sinoatrial node and allowing other electrical influences to predominate. A further factor that adds to this is a long refractory period between beats, i.e. a low resting heart rate. More time between the 'good' electrical impulses gives the 'bad' electrical impulses time to get something going. Indeed, Grimsmo et al. found that very low resting heart rates were associated with AF in elite cross-country skiers.
Interestingly, Coumel goes one step further to categorize a-fib into 2 distinct forms - a vagal form and a sympathetic form, with the sympathetic form being more typical of 'old age onset a-fib' and the vagal form typically being more common to athletes and occuring more often when vagal tone predominates when the athlete is relaxed - at night, rarely during physical or emotional stress and often preceded by bradycardia (slow heart rate). Interestingly, this has been my experience with incidences of a-fib, i.e. they are most noticeable at night when I am sitting on the couch and more rare during exercise.
It seems like a fair conclusion, then, that endurance training increases the risk for a-fib, possibly through multiple channels, so what should we do about that?
In the last few years, the link between long term endurance training and arrhythmia risk has hit the mainstream media and, predictably, been exaggerated and sensationalized to the point that it is scaring some away from long term aerobic exercise. My good friend, & blogger on athlete heart issues, cardiologist, Dr. Larry Creswell (www.athletesheart.org) helps to keep this in perspective - "the rewards of regular training still far outweigh the risks" & his thoughts are 100% backed up by mortality studies that show the overall positive influence endurance training has on longevity even at VERY high levels (e.g. Tour De France cyclists).
In my own experience with a-fib, the importance of all of that other 'good stuff' that long term aerobic exercise brings has been made clear. After going through a bunch of varied tests, despite the discovery of this heart condition, the advice of the Doc as to what we should change is, at this point, not much! As I said above, the primary risk of a-fib among the general population is increased risk of stroke. Athletes, on the whole, have very low risk of stroke (& other cardiovascular events) based on the other positive factors that endurance training brings, i.e. good cholesterol numbers, good blood pressure, good blood glucose numbers etc. Additionally, even the primary problems with sustained a-fib (i.e. a tired heart!) are significantly mitigated due to improved fitness. A well trained athlete who has a large stroke volume & maybe a heart rate of 60 while walking has a lot more room to play with, in the case of an a-fib episode, than someone who may already be at 120 under normal conditions! While the ordinary age-related onset of a-fib is generally accompanied by other issues, this 'young onset' variation without accompanying conditions (sometimes called 'lone' a-fib) appears to be relatively benign and still a bit of a mystery as to how (if) it will lead to any other problems.
There have been few really long term studies of a-fib progression/prognosis generally and even less in athletes, but the research seems to be heading in the direction of - it's hard to predict. For example, in one of the longest studies on a-fib progression, only ~40% of cases progressed from paroxsymal ('come and go') a-fib to persistent a-fib over the course of 6 years. In another ~4 year study, ~40% had no recurrence, ~40% remained in paroxsymal a-fib and ~20% progressed to 'persistent' a-fib
So, for the time being, I am taking a low-dose aspirin a day to decrease the risk of a clot forming but continuing to exercise as normal. The only change in that regard is if I feel an a-fib episode coming on, I will slow to a walk until it dissipates. Hardly a major issue. I see it as my body reminding me that it may be time to stop and smell the flowers every once in a while :-)
More advanced treatment options usually involve beta blockers to slow the heart coupled with more heavy-duty blood thinners such as Warfarin or cardiac ablation - a procedure to burn off the faulty tissue that is causing the 'short circuit'. While beta blockers don't appeal due to my relationship with exercise, I will consider ablation if the bouts become more persistent. Regarding ablation, an important thing to note is that according to Tutuianu et al. (2015)the success of the procedure, particularly a single procedure, goes down after the a-fib moves from paroxsymal (temporary) to persistent. Ablation when paroxsymal resulted in 61% remission at 3 years vs only 41% when the condition had progressed to persistent before ablation. That said, multiple ablations increased this to a 77% success rate. So, to me it's a bit of 'bet-hedging' on the likely progression of the condition vs the potential need for multiple ablations in the future.
In retrospect, what would I have done differently?
I should add the standard disclaimers at this point. I am an exercise physiologist, not a Doctor. Take my perspective purely as my perspective. If you're having issues you should chat with a cardiologist.
While the understanding of this condition, especially athletic contributors to this condition, is very much still in the formative stage, I suspect that we will find that, like most health issues, stress coupled with inflammation and incomplete recovery/healing plays a large role. Already the increased incidence of fibrosis in trained arrhythmic hearts would point to this as an important factor. In this sense, it may be fair to conclude that rather than the cardiac stress itself, incomplete recovery/healing from the stress & or sustained inflammation plays an important role. I can certainly think back to doing dumb things like training & racing while ill and training when my body was clearly in a state of inflammation and requesting recovery. I suspect these instances may play a disproportionate role in the development of a-fib. If talking to my younger self, I would advise him to err on the overly cautious side when coming back from illness or big load. On a related note, because Heart Rate Variability is one of the best and easiest ways to monitor the body's inflammatory state, I would also advise him to begin monitoring his HRV (& acting in accordance with it) much earlier in his athletic journey.
One thing that I did do right was to recognise the importance of an 'extended break' or unloading period each year. Furlanello et al. (1998) found that in a number of cases, among elite athletes, a-fib can be treated by simply inserting a deliberate, extended period of detraining/recovery.
While I will keep posting here as my experience progresses and I continue to learn about the condition, my current conclusions would be
* If you live long enough, chances are pretty good that you will develop a-fib at some point.
* If you are a serious endurance athlete, this process is likely sped up in accordance with your lifelong training volume.
* But, if you are an endurance athlete, many of the more serious (deadly!) problems associated with a-fib (stroke, heart failure etc) are strongly mitigated due to your improved fitness and metabolic health.
* So, despite my recent experience, in a risk/reward sense I still firmly believe that a large amount of aerobic activity is a VERY good thing for your overall health & I plan to continue adding to my lifetime beats tally! :-)
Just be sure to...
Train smart,
AC
TweetDon't miss a post! Sign up for my mailing list to get notified of all new content....